Introduction:
Urgent care is a challenging, yet fascinating scope evidenced by the myriad of cases that come through the doors. Knee injury is a common presentation. A thorough history and physical examination is imperative to exclude any internal derangements to the knee. At this stage, it is important that a differential diagnosis is postulated. The use of fast scan in an urgent care setting is becoming popular. In this paper, emphasis is placed on the clinical acumen in diagnosing anterior cruciate ligament (ACL) structural integrity using good clinical examination skills and bedside ultrasonography.
Search engine used: PubMed and Google Scholar. Keywords: ACL injury, Clinical Examination, Bedside ultrasound.
Case Description:
Demographics: 36 years old Samoan male. Presented himself to urgent care clinic 24 hours after injury.
Presenting Complaint: Presents with right knee injury– painful and swollen. Limping and sore to bend his knee.
History of Presenting Complaint: Tackled by an opponent on his inner knee while playing rugby. Developed an immediate pain and was unable to continue playing. Swelling was reported within a few hours with reduced range of motion (ROM). Iced his knee on the day of injury and took some paracetamol.
Past Medical History: Normally fit and well. Previous right shoulder operation. Nil regular medications. No known drug allergies.
Examination: Antalgic gait. Right knee – joint effusion and medial joint line tenderness. ROM 45-100 degrees. Tender medial collateral ligament (MCL) on stressing. Examination was difficult due to pain and guarding but anterior/posterior drawer test/ Lachmann’s test felt intact with an end point. McMurray’s test not done due to acute presentation. Neurovascular status intact.
Investigation: Xray showed no dislocation or fracture. Suprapatellar knee joint effusion present on X-ray lateral view. No lipohaemarthrosis.
Impression: High suspicion of ACL injury with associated medial meniscus and MCL involvement.
Management: Accident Compensation Corporation (ACC) form completed. Given time off work. Analgesia (Paracetamol 1 g QID/PRN and Ibuprofen 400 mg TDS/PRN) prescribed. Patient put in Zimmer splint and advised partial weight bearing with crutches. He was referred to the Sports Clinic for further assessment within 48 hours. He was referred for an MRI which showed a complete anterior cruciate ligament (ACL) rupture with associated medical meniscus tear. He underwent ACL rehabilitation under the Sport and Exercise Physicians supervision for a month and was eventually referred to orthopaedics for an ACL reconstruction.
Case Discussion:
Anterior Cruciate Ligament Anatomy and Biomechanics:
Anterior cruciate ligament (ACL) injury is a common presentation with the prevalence of 4% of adults presenting to primary care with acute knee pain(1). The ACL is a dense connective tissue structure that runs from the anterior tibial spine to the femoral condyle. It has a length of approximately 3cm and a width of 1cm on average(2). It is made up of two main components: the anteromedial and posterolateral bundle(2). The microstructure of the bundles is mainly made up of type 1 collagen and matrix (glycoproteins, glycosaminoglycans, elastin)(2). It is innervated by the posterior articular branches of the tibial nerve and gets it blood supply from the branches of the middle genicular artery(2). The ACL plays a role in knee stability by preventing anterior tibial translation and resisting multiaxial and rotational forces. Certain sports such as skiing, football and rugby run a higher risk of ACL injury(3). A high amount of ACL injuries is non-contact, with the foot planted on the ground and the knee semi-flexed. At this point, the ACL is taut and is vulnerable to rupture or avulsion injury due to the large forces that travel through the knee joint. Risk factors for ACL injury can be categorized as either extrinsic or intrinsic.
Intrinsic risk factors for ACL injury include(4):
- having decreased intercondylar notch width on plain radiography; and
- developing increased knee abduction moment (a valgus intersegmental torque) during impact on landing.
Sonnery-Cottet et al. in their paper suggest that an increased posterior tibial slope and a narrow tibial notch width increases the risk of an ACL injury(5). Valgus collapse positions leads to ACL shortening(6). This position can be mimicked with the knee in 30 degrees flexion, internally rotating the hip and external tibial rotation, thus putting the knee at high risk of ACL injury(6). Knee adduction moment is at its highest when landing from a jump position(6). Emphasis should be placed on the importance of dynamic loading of the knee joint through proprioception and neuromuscular training(4). Techniques of landing softly on both the forefoot then rolling backward with involvement of both knee and hip flexion(4). As stated above, it is important to avoid excessive valgus loading of the knee. An often advised technique would be the “knee over toe position” when making sudden cutting or change in position(4).
Extrinsic risk factors for ACL injury include(4, 7, 8):
- Type of sport
- Coefficient ratio between playing surface and shoes
- Weather conditions
There are also extrinsic risk factors that could play a part in higher rates of ACL injury. The paper by Paterson K.L. et al. studied the barefoot landing of a small number of women versus stability of using shoes (7). The result showed that stability with appropriate footwear improved knee biomechanics and reduced the chances of an ACL injury (7). In another study done by Renstrom P. et al. and colleagues argue that although increasing the coefficient between the playing surface and sports shoe may improve traction contact and enhance performance, it has several ramifications, i.e. higher risk of ACL injury (4). Intuitively sports athletes prefer higher shoe-surface traction interface. As discussed above, the downside of this is the higher risk of ACL injuries, especially with a foot planted on the ground. The force that goes through the knee joint is multifaceted. The high levels of rotational traction or torque presents a higher risk of an ACL injury (8). A meta-analysis by Thomson A. et al. presented three prospective studies looking at shoe-surface traction and ACL injuries (8). Subtle changes in playing surface area requires appropriate foot wear due to the changes in friction coefficient playing surface(8). Interestingly , meteorological conditions is also a factor in risk of sustaining ACL injury (4). Low rain fall and the subsequent evaporation increase the risk of non-contact ACL injury by increasing the shoe-surface traction coefficient (4).
Evidence on Clinical Examination and Bedside Ultrasonography:
Historically , literature suggest that the accuracy of ACL diagnosis at the first medical consult is poor(3). A paper by H. Parwaiz and colleagues showed that less 10% of patients with ACL injuries are diagnosed at first physician consult and the average delay from first presentation to diagnosis is approximately 21 months(9, 10). Missing ACL injuries can have detrimental effects with cartilage damage and meniscal tears and development of premature knee osteoarthritis(1). There are often other associated structure damage in the knee especially the medial meniscus which is usually picked up later on MRI(3). In his paper, H. Parwaiz showed that primary care physicians were able to detect about 60% of chronic ACL injury compared to about 90% by an orthopaedic surgeon(9, 11). This was also supported by the paper by Geraets, Stijn E.W. et al. which showed orthopaedic surgeons recognized 94% of ruptured ACL through a medical history and physical examination compared to primary care physicians at only 62% (11). Another finding from this study was physical examination did not confer any additional benefit to primary care physicians (11). There are two plausible explanations for the misdiagnosis of ACL injury. Firstly, primary care clinicians lack the necessary skill or training in diagnosing ACL injury(9). Secondly the acute presentation of a swollen and painful knee makes it difficult to discern differences between both knees(9). Clinical examinations are subjective and often made difficult due to muscle spasm and discomfort elicited during examination(12). Several studies have shown in the past the poor yield in examination findings for the acute painful knee. To date, there is no convincing research that studied the role of knee joint aspiration in the acute setting. A retrospective cohort study carried out in South Korea showed that knee joint aspiration for acute haemarthrosis in the emergency department (ED) setting helped reduce pain levels, improve range of motion and clinical examination (13). This was a small study that looked at 60 patients in the emergency department setting. They were divided into two groups, presence versus absence of knee aspiration in the acute setting. The patients were also followed up in the outpatient clinic within one to two weeks. The study suggested that removing fluid from the knee joint helped diagnose the presence intra articular pathology, i.e. if knee joint aspirate shows presence of fat layer this most likely involves an occult fracture (13). Anecdotally, removing fluid from the knee joint will reduce pressure exerted on the nerve fiber mechanoreceptors and therefore, reducing pain signal transmission via nerve endings (13). Although this was a small study and lacked the relevant scientific data, it showed substantial decrease in pain levels and increase in sensitivity of clinical examination i.e., Lachmann and pivot shift test during the second clinic follow up. But is this good enough and is there still a need for improvement of our skills in diagnosing internal knee injuries as the number of musculoskeletal injuries increase with the growing population?
A systematic review by Swain M.S. et al. studied the diagnostic accuracy of clinical tests for the diagnosis of ACL injury(1). A total of 285 studies were looked at with only 14 studies included in descriptive synthesis due to clinical heterogeneity (1). One of these studies was carried out in a primary care setting. They examined five key points in the history i.e. effusion, popping sound at time of injury, pain, instability/give way, and inability to continue playing, and four clinical signs from physical examination i.e. anterior drawer test, Lachman’s test, prone Lachman’s test and pivot shift test (1). Although the pivot shift test is a much more sensitive clinical test compared to anterior drawer and Lachmann’ s test, it causes significant discomfort and muscular spasm which makes it difficult to examine the acutely injured knee (14). Consensus from the paper was clinicians should not rely on individual history items and physical examination tests in isolation due to the poor diagnostic accuracy for ACL injury, nevertheless there is benefit to combining clinical tests which have higher diagnostic value(1). Although this was a systematic review, the study acknowledged that the major drawback was that the studies was not quantitative and were low power to analyse multiple studies (1). The Dutch orthopaedic guidelines in 2011 recommended combining medical history taking with the anterior drawer test, Lachmann’s test and pivot shift test to optimize the finding of ACL rupture (11). Another systematic review published in 2014 by Toni Lange and colleagues looked at clinical examination of the knee for ACL integrity (15). There were 110 articles on the initial search which subsequently was narrowed down to seven articles meeting the inclusion criteria (15). Again, the Lachmann test specifically in the prone position scored the highest intra rater reliability (15). The conclusion from the study was systematic studies on the reliability of physical examination tests for assessing the ACL integrity are limited and of varying levels of methodological quality (15). This begs the question, should we be using bedside ultrasonography in our practices for knee injuries to help improve our ACL injury detection accuracy? What does the literature say about this?
The Use of Bedside Ultrasonography:
The scarcity of literature on the use of bedside ultrasonography in the acute knee setting makes this a debatable and interesting topic of discussion. Even more so in this day and age, more urgent care doctors (primary care clinicians) are utilizing bed side ultrasound to assist with achieving an accurate diagnosis. However, is this justifiable? Ultrasound is well accepted for evaluating extra-articular knee structures but its role and effectiveness in evaluating intra-articular structures is debatable (16).
There are several papers published on the use of ultrasound in diagnosing ACL injury. Although Magnetic Resonance Imaging (MRI) is widely considered the gold standard for non-invasive investigation of ACL injury, its cost, time and availability are the main factors for limiting universal use (16). Conversely, ultrasound is a cheaper modality with easier access. In New Zealand, an MRI requires a referral from an orthopaedic surgeon or sports physician which is covered by ACC. The whole process of seeing an urgent care doctor and subsequent referral to a specialist and then for an MRI involves time. There is delay from diagnosis to treatment, be it be structured rehab or surgical reconstruction. This paper will mainly examine the use of bedside ultrasonography in an urgent care (primary) care setting where bedside ultrasound is fast becoming a trend.
A study carried out in India by a group of orthopaedic surgeons Kumar S. et. al. examined 130 patients in an outpatient setting (16). They used ultrasound imaging on both knees and compared it with MRI findings. Patients were asked to lie prone with their knees in 20-degree flexion. Sagittal views were obtained of the femoral and tibial condyles. Reference lines were then drawn tangent to the condyles. Anterior pressure was applied to the tibia to check for anterior translation. An average of three measurements were obtained. This was compared with the uninjured knee. A shift of 1mm or more between the knees was considered positive (16). The results were then compared with MRI findings. The results were reassuring with a sensitivity of 86% and specificity of 89% (16). The downside to this study was that the study was done on follow up patients in an outpatient setting. The patients would have had some sort of rehab and may have continued with their activities of daily living. This would have created secondary self-protective mechanisms by the surrounding ligaments, tendons, and muscles. The other limitation of the study was the scans were done by a single radiology consultant. The study says it cannot safely conclude if the results can be reproduced since it is user dependent (16).
In 2009 Palm H.G. and colleagues published a paper which suit the urgent care model. They studied acute ACL injuries (14). The study consisted of 33 patients. An examiner without specialist skills was trained for a short period of time. The objective of the study was to determine if an examiner without specialist knowledge in ultrasound could accurately diagnose acute ACL injury using bedside ultrasonography (14). This study is applicable in the urgent care setting where an urgent care physician examines and does ultrasonography to accurately diagnose ACL injuries. As with the previous study, Palm H.G. studied the differences between the injured and uninjured knees. Reference lines were drawn from the femoral condyle to posterior tibia. Manual pressure was then applied ventrally onto the tibia. An anterior tibial translation of 1 mm or more was considered positive for an ACL rupture (14). This prospective study highlighted that ultrasound had good sensitivities in detecting ACL injuries well above 90% (14). The paper concluded that a clinician without specialist skill could be easily be trained to accurately diagnose acute ACL injuries using bedside ultrasonography (14). It is a painless and fast procedure which works well in a primary care or small hospital setting (14).
Grzelak P. et al. and colleague also studied ultrasonography use in acute knee injury (12). They had their patients sit up in supine position and measured differences in anterior translation of the knee joint (12). They used a threshold of 2 mm side to side difference between injured and uninjured knees, and/or absolute difference of 5mm or more as a positive marker of ACL injury (12). This gave the ultrasonography method a sensitivity of 91.5% and a specificity of 95.6% (12). Again, a high sensitivity and reliable modality for detecting ACL injury. In the study, it highlighted that despite MRI being the gold standard of investigation for ACL injuries, it is not as effective on patients with metallic implants. Furthermore, it does not provide additional information on mechanical or functional joint stability (12). On the other hand, ultrasound is more flexible and allows dynamic range of motion in a quantitative manner (12). Zaka Khan et al. published a paper on the use of ultrasound in the assessment of internal derangement of the knee (17). The looked not only at ACL injuries but also the posterior cruciate ligament (PCL), medial collateral ligament (MCL) and lateral collateral ligament (LCL) with use of ultrasonography. The current non-invasive gold standard investigation for knee injury is MRI and arthroscopy as gold standard invasive test (17). This was a double blind prospective study which included 60 patients (17). The study managed to demonstrate that ultrasound yields high sensitivity and specificity. The writer confidently acknowledged although this is a learning curve, ultrasound should be used a screening tool before MRI or when clinical examination is difficult (17).
In a nutshell, a patient who presents with suspected ACL injury, bedside functional ultrasonography is a quick and reliable imaging to diagnose ACL injury. It is readily available and requires minimal user training. Ultrasound has the ability to combine dynamic clinical examination with real time visualization (12). Nonetheless, MRI is still the imaging of choice to further elaborate structures injured in the knee, albeit later in management. In my opinion, ultrasound will not and should not replace MRI. It is safe to say, that if clinical examination and ultrasound yield negative results for ACL injury, then MRI is not indicated. If ultrasound is suggestive for an ACL injury, then MRI is indicated to evaluate other structures in the knee. This will curtail unnecessary MRI referrals and reduce cost and delay of treatment.
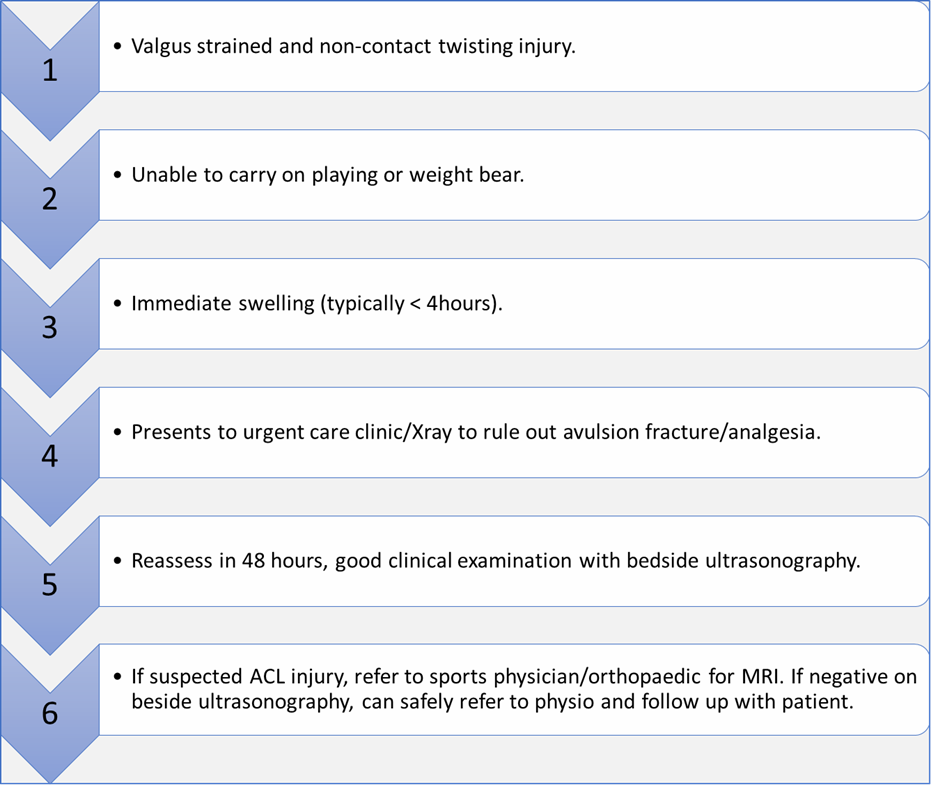
Below is a proposed flow chart from diagnosis of ACL injury to specialist referral:
Conclusion:
Although there is a dearth of literature on anterior cruciate ligament, there are still a few schools of thought in terms of clinical diagnosis and the use of ultrasonography in primary care. As elaborated earlier, although MRI is the gold standard for non-invasive ACL diagnosis, good ultrasound skills is an inexpensive and reliable modality for ACL diagnosis. There is a clinical realm to educate urgent care and ED physicians to improve their clinical skills e.g., anterior drawer test, Lachmann’s test and pivot shift test. Nevertheless, improving diagnostic accuracy with use of these clinical tests may not be necessarily helpful in the acute setting of an injured knee (3). This research has encouraged me to acquire more knowledge on bedside ultrasonography for acute knee injuries and to hone my ultrasound skills to allow quicker and accurate diagnosis of acute knee injuries.
REFERENCES:
- Swain MS, Henschke N, Kamper SJ, Downie AS, Koes BW, Maher CG. Accuracy of clinical tests in the diagnosis of anterior cruciate ligament injury: a systematic review. Chiropractic & manual therapies. 2014;22(1):25.
- Duthon VB, Barea C, Abrassart S, Fasel JH, Fritschy D, Menetrey J. Anatomy of the anterior cruciate ligament. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2006;14(3):204-13.
- Arastu M, Grange S, Twyman R. Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(4):1201-5.
- Renstrom P, Ljungqvist A, Arendt E, Beynnon B, Fukubayashi T, Garrett W, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. British journal of sports medicine. 2008;42(6):394-412.
- Sonnery-Cottet B, Archbold P, Cucurulo T, Fayard J-M, Bortolletto J, Thaunat M, et al. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. The Journal of bone and joint surgery British volume. 2011;93(11):1475-8.
- Utturkar G, Irribarra L, Taylor K, Spritzer C, Taylor D, Garrett W, et al. The effects of a valgus collapse knee position on in vivo ACL elongation. Annals of biomedical engineering. 2013;41(1):123-30.
- Paterson K, Sayer T, Bennell K, Hinman R, Bryant A. The effects of stability footwear on ACL-relevant knee biomechanics during landing in women. Journal of Science and Medicine in Sport. 2015;19:e60.
- Thomson A, Whiteley R, Bleakley C. Higher shoe-surface interaction is associated with doubling of lower extremity injury risk in football codes: a systematic review and meta-analysis. British Journal of Sports Medicine. 2015;49(19):1245-52.
- Parwaiz H, Teo AQ, Servant C. Anterior cruciate ligament injury: A persistently difficult diagnosis. The Knee. 2016;23(1):116-20.
- Bollen SR, Scott BW. Rupture of the anterior cruciate ligament — a quiet epidemic? Injury. 1996;27(6):407-9.
- Geraets SEW, Meuffels DE, van Meer BL, Breedveldt Boer HP, Bierma-Zeinstra SMA, Reijman M. Diagnostic value of medical history and physical examination of anterior cruciate ligament injury: comparison between primary care physician and orthopaedic surgeon. Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(4):968-74.
- Grzelak P, Podgórski MT, Stefańczyk L, Domżalski M. Ultrasonographic test for complete anterior cruciate ligament injury. Indian journal of orthopaedics. 2015;49(2):143-9.
- Wang JH, Lee JH, Cho Y, Shin JM, Lee BH. Efficacy of knee joint aspiration in patients with acute ACL injury in the emergency department. Injury. 2016;47(8):1744-9.
- Palm H-G, Bergenthal G, Ehry P, Schwarz W, Schmidt R, Friemert B. Functional ultrasonography in the diagnosis of acute anterior cruciate ligament injuries: a field study. The Knee. 2009;16(6):441-6.
- Lange T, Freiberg A, Dröge P, Lützner J, Schmitt J, Kopkow C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture – A systematic review. Manual Therapy. 2015;20(3):402-11.
- Kumar S, Kumar A, Kumar S, Kumar P. Functional Ultrasonography in Diagnosing Anterior Cruciate Ligament Injury as Compared to Magnetic Resonance Imaging. Indian journal of orthopaedics. 2018;52(6):638-44.
- Khan Z, Faruqui Z, Ogyunbiyi O, Rosset G, Iqbal J. Ultrasound assessment of internal derangement of the knee. Acta orthopaedica belgica. 2006;72(1):72.
