In the early 1990’s, the American College of Sports Medicine (ACSM) issued a model called the Female Athlete Triad. It was proposed as part of the Task Force on Women Issues.
Its initial target was sports that emphasized on aesthetics or lower total body mass such as gymnastics, running and skating. There was higher incidence of disordered eating as compared to the general female population.
The old school of thought of the Female Athlete Triad was made up of a simple understanding of energy deficiency in athletes. It looked at disordered eating/eating disorder and its effects on menstrual cycle and bone health in female athletes(1). It has three distinct factors: disordered eating, amenorrhoea and osteoporosis.
An updated version took into account a wider range of factors, i.e. low energy availability/disordered eating, amenorrhoea/menstrual disturbances and osteoporosis/bone loss.
The triad was expanded a few times from its binary version.
How Does RED-S Differ from Female Athlete Triad?
The International Olympic Committee (IOC) worked on a broader, multifactorial and more complex term from the previously known “Female Athlete Triad”. Although in its “infancy stage”, it also included male athletes.
Umbrella term = Relative Energy Deficiency in Sports (RED-S)(2).
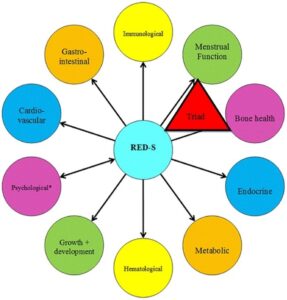
Relative Energy Deficiency in Sports (RED-S) is a model proposed with complex interaction of physiological factors with a causal link of low energy availability. It suggests that rather than working on three separate entities, it is a continuum of spectrum that affects physiological function, health and athletic performance. Energy deficiency is caused by relative energy intake to energy expenditure required for physiological function, activities of daily living, sports and growth. This involves a myriad of physiological functions such as metabolic rate, immunity, bone health, cardiovascular health, menstrual health and protein synthesis. These are all somehow interrelated.
There is caveat however, some feel the RED-S is not suitable as it does not involve the three primary factors, but instead involves multiple other additional considerations. A paper by De Souza and colleagues scrutinized the IOC paper and stated that RED-S should be looked at scrupulously(2).
RED-S Conceptual Framework:
It is a build and elaboration on the symptoms discussed in the Female Athlete Triad Model:
Being an athlete requires sufficient energy availability to allow for normal physiological cellular function. Energy Availability(EA) is Energy Intake(EI) less Exercise Energy Expenditure(EEE). A person requires at least 45 kcal/kg of fat free mass(FFM) for normal muscle protein synthesis per day. Low energy availability (LEA) leads to the body conserving energy by making adjustments to bodily systems by disrupting an array of metabolic, hormonal and functional processes. Adequate energy availability is essential for normal ovulatory cycle and menstruation to occur. It is plausible that bone health is affected by the availability of sufficient energy. Estrogen helps with the uptake of calcium into the blood circulation and subsequent deposition into bone whereas progesterone facilitates this function through a few complex mechanisms. Ergo, any imbalance in estrogen/progesterone will affect bone health. For females, peak bone mineral density is achieved around 19 years of age and 20.5 years for males.
Hormonal Imbalance and Menstrual Cycle:
Eumenorrhoea – regular menstrual cycles occurring at an interval of 21 to 35 days.
Primary amenorrhoea- failure to establish menarche by the age of 15 years old.
Secondary amenorrhoea- absence of 3 consecutive cycles post menarche.
Secondary amenorrhoea prevalence can be as high as 65% in runners.
Low EA can lead to LH pulsatility reduction (low GnRH from hypothalamus) which is required for normal menstrual cycle. This affects the hypothalamic pituitary axis (HPA). Known as Functional Hypothalamic Amenorrhoea (FHA).
Are male athletes at risk too? Research applicability?
Although most of the literature on low EA focus on female athletes, low EA in males tend to occur at the same at risk sports as females, especially at sport competitions where weight and leanness are important for the role in performance, appearance and meeting the competition weight category. Prevalence in elite male athletes is high especially in cycling, gravitational sports and non weight bearing sports e.g. jockey, endurance runners, cycling(3).
Albeit simple formulae have been provided in some studies for low unsafe EA in athletes, there are some caveats to this. The complex dose-response relationship between reduction in EA and disruption in various hormones and bone formation markers vary in nature and thresholds amongst athletes. Also findings in a laboratory setting may not be applied directly to athletes competing outdoors. There are also numerous other variables that may affect directly or interact with one another such as psychosocial stress, dietary characteristics etc.
Health & Performance Consequences:
When an athlete trains hard, they require higher nutrient intake to maintain normal energy homeostasis. Whilst the body is able to adapt this over a short period, over a long period, low energy availability leads to reduced performance. RED-S can have serious implications to health over long-term and causes premature reduction in physical, psychological and mental capacity. Over time, low EA can lead to nutritional deficiencies leading to anaemia, chronic fatigue and low immune status leading to infection susceptibility.
It affects different systems(4):
CVS- impaired endothelial vasodilation (downregulation of NO), lipid dysfunction (higher total cholesterol and LDL).
Gastrointestinal (GI)
Endocrine- reduced growth hormone production, slowing of metabolic rate. Increased pro-inflammatory markers such as Interleukin-6 and Apolipoprotein-B.
Reproductive- disruption of menstrual cycle/Functional Hypothalamic Amenorrhoea, ED. Testosterone has anabolic effects on bones. Low testosterone leads to low BMD in males.
Skeletal- impaired perfusion to working muscles, impaired oxidative metabolism, stress #, osteopenia, peak bone mass F 19, M 20.5 yo. Oestrogen helps uptake of calcium into blood and deposition into bones and progesterone facilitates this by multiple complex mechanisms. High risk fractures such femoral neck , metatarsal bones.
Renal- aneamia
Psychological- stress, depression, anxiety, poor self esteem, poor concentration and training response
Immune – susceptible to viral illnesses
Poor exercise performance and response to training.
SCREENING for RED-S:
Having a model like RED-S allows practical application and transferable framework for diagnosis and treatment(5). Athletes need to be screened and educated individually on EA and the deleterious outcomes of LEA on health and performance. There is still a lack of standardized method for measuring EA and the information on injury and CVD risk in the state of relative energy deficiency.
Screening for RED-S should be part of an annual health examination for athletes. Early detection is important and to prevent the long term consequences of energy deficiency. No consensus yet on the best screening tool in terms of efficacy.
Functional clinical assessment tool called RED-S CAT is a framework used to guide athletes back to return to play. It uses a simple return to play rating that clinicians can use to help athletes return safely to sporting competition(6).
EA (kcal/kg FFM/day)= EI (kcal/day) – EEE(kcal/day)
Ideally EI and EEE can be measured over a period time that is representative of habitual practice.
Dual Energy X-ray absorptiometry (DXA) and anthropometry can be utilized for FFM measurement.
Brief Eating Disorder in Athletes Questionnaire (BEDA-Q) is a screening tool used in female athletes to distinguish between with/without ED.
Eating Disorder Examination 16 (EDE-16)- semi structured interview
Get a good menstrual history – age menarche, regularity of menses, medication use, sexual history (rule out pregnancy), family menstrual history. A full physical examination +/- pelvic examination.
Blood test- FBC, TSH/T4, FHS/LH, Prolactin, Oestradiol, HCG, Androgen profile
Biomarkers for LEA such as Leptin/T3/Cortisol can be used but weak evidence to date.
Consider DEXA scan if amenorrhoeic of >6 months. A Z-score value of < 2.0 with secondary clinical factors is considered osteoporotic.
Treatment of RED-S
Treatment can involve increase in EI, reduction in exercise or combination of both. Requires a multidisciplinary health support team which includes a sports physician, psychologist, dietitian and coach.
Some scientific studies done on addition of energy rich supplement between meals and introduction of rest day to weekly training programme.
A practical approach may be implementing a diet plan that increases EA by 300-600 kcal/day and address any energy deficiencies throughout the day and around exercise sessions. Treatment of LEA by increasing caloric intake and/or reducing exercise energy expenditure is preferred over hormonal therapy.
Reestablishing menstrual cycle-a reliable predictor is weight gain. Adequate carbohydrate and protein intake is required to replenish liver glycogen stores and stimulate LH pulsatility.
Macronutrient intake– High carb diet should be promoted. Most athletes have a low carb diet and high in fiber. This could be due to media drive fat free diet trends such as paleo and gluten free diets.
Micronutrient intake– Vitamin A/C/D/E/K, Riboflavin, Folate, Calcium, Zinc, Iron, Magnesium
Many physicians prescribed low dose oral contraceptives in amenorrhoeic athletes, although this does not correct the underlying aetiological cause of relative energy deficiency.
Optimise bone health– mechanical loading and high impacts loading training should be implemented for at least 2-3 days/week for athletes with decreased BMD. This will improve mineralization of trabecular bone and growth of cortical bone. A diet consisting of calcium 1500 mg /day and Vit D 1500 IU/day is recommended.
Behavioral interventions- psychological input from mental health clinicians. Treat any pathological eating behaviours such as purging, laxative abuse, eating disorder (anorexia nervosa, bulimia nervosa, anorexia athletica).
Avoid alcohol and smoking.
The Sports Risk Assessment and Return to Play model has subdivided into three groups and provides appropriate advice for the safety of return to sport.
Green rating- athlete is safe to return to full return to play and has a healthy and appropriate body weight.
Yellow rating- caution should be applied. Close watch on athlete is required. Energy input, output and training load should be assessed. Athlete can continue to train as long as following treatment plan but return to play can only be cleared by a medical staff. Reevaluation can take place in 1-3 months.
Red rating – athlete requires immediate medical attention. No training or competition should take place. Use of written contract.
Reference:
- Mountjoy M, Sundgot-Borgen J, Burke L, Ackerman KE, Blauwet C, Constantini N, et al. International Olympic Committee (IOC) consensus statement on relative energy deficiency in sport (RED-S): 2018 update. International journal of sport nutrition and exercise metabolism. 2018;28(4):316-31.
- De Souza MJ, Williams NI, Nattiv A, Joy E, Misra M, Loucks AB, et al. Misunderstanding the female athlete triad: refuting the IOC consensus statement on Relative Energy Deficiency in Sport (RED-S). BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2014.
- Tenforde AS, Barrack MT, Nattiv A, Fredericson M. Parallels with the female athlete triad in male athletes. Sports Medicine. 2016;46(2):171-82.
- Logue D, Madigan SM, Delahunt E, Heinen M, Mc Donnell S-J, Corish CA. Low energy availability in athletes: a review of prevalence, dietary patterns, physiological health, and sports performance. Sports Medicine. 2018;48(1):73-96.
- Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC relative energy deficiency in sport clinical assessment tool (RED-S CAT). BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2015.
- Statuta SM, Asif IM, Drezner JA. Relative energy deficiency in sport (RED-S). Br J Sports Med. 2017;51(21):1570-1.
