By Rohil V Chauhan, Amanjeet Toor, Anand H Segar
Lower back and buttock pain in older adults is often attributed to lumbar or hip degenerative pathology. However, in patients with multimorbidity, particularly those with malignancy or osteoporosis, broader causes must be considered.
We present a 71-year-old female with three episodes of intractable, alternating buttock pain over 12 months, diagnosed with bilateral sacral insufficiency fractures (SIFs) upon orthopaedic consultation. This case illustrates the diagnostic challenge of SIFs and the importance of multi- disciplinary management in fragility fracture care.
Case-Presentation
A 71-year-old woman was referred to a secondary care orthopaedic spine clinic following three episodes of severe buttock pain over 12 months without an injury mechanism. The first two episodes involved the left buttock, and the most recent affected the right. Each episode lasted 3–5 weeks, significantly impairing mobility and function, but resolved without medical consultation. She was asymptomatic at the time of orthopaedic review; however, her general practitioner referred her due to a history of vertebral fragility fractures and multiple recurrences. Her medical history included hypertension (managed by amlodipine), osteoporotic vertebral fractures at L3 (approximately 70% vertebral height loss) and T12 (approximately 30% loss) and early-stage rectal cancer treated with low anterior resection and ostomy reversal in 2020, with no recurrence to date. She also had essential thrombocythaemia and myelodysplastic syndrome, managed with a stem cell bone marrow transplant in 2023, and remained under haematology care.
On examination, lumbar range of motion was full and non-provocative. Tandem gait and Romberg’s sign were unremarkable. There was mild focal tenderness over the superior left sacroiliac joint. Hip and sacroiliac joint provocation tests were negative bilaterally. Neurological Assessment of the lower limbs revealed intact power and light touch sensation, with brisk (3+) deep tendon reflexes and no long tract signs. Lumbar spine radiographs (Figure 1) confirmed chronic vertebral compression deformities at L3 and T12. Given her fragility fracture history, cancer background and symptom severity, lumbosacral magnetic resonance imaging (MRI) was arranged to assess for occult pathology. MRI revealed multilevel lumbar spondylosis with left-sided L5 and S1 nerve root compression. Notably, MRI also demonstrated bilateral sub chondral bone marrow oedema in the sacral alae, consistent with recent SIFs (Figure 2B).
Given the absence of pain, surgical or interventional management was not indicated. She was referred to endocrinology for osteoporosis evaluation and to physiotherapy for a rehabilitation programme focused on gradual, low intensity strength and balance training.
Discussion
This case highlights several considerations in the evaluation of lumbopelvic pain in older adults with multimorbidity. SIFs are frequently under-diagnosed, particularly when plain radio graphs are unremarkable. The sacrum is often inadequately visualised on standard lumbar radiographs, and clinical presentation may mimic more prevalent causes of axial or radicular pain. MRI, particularly T2-weighted coronal lumbosacral and coronal oblique sacral sequences, offers high sensitivity (near 100%) in detecting SIF-associated early marrow oedema. The patient had multiple established risk factors for fragility fractures, including established osteo porosis, prior vertebral compression fractures, malignancy and recent stem cell transplantation.
Figure 1: Lateral lumbar extension radiographs demonstrate a chronic anterior wedge compression deformity of L3, with approximately 70% loss of vertebral body height. A similar but less severe compression deformity is noted at T12 (approximately 30% loss). There is also grade 1 anterolisthesis of L4 on L5 due to degenerative spondylolis thesis.
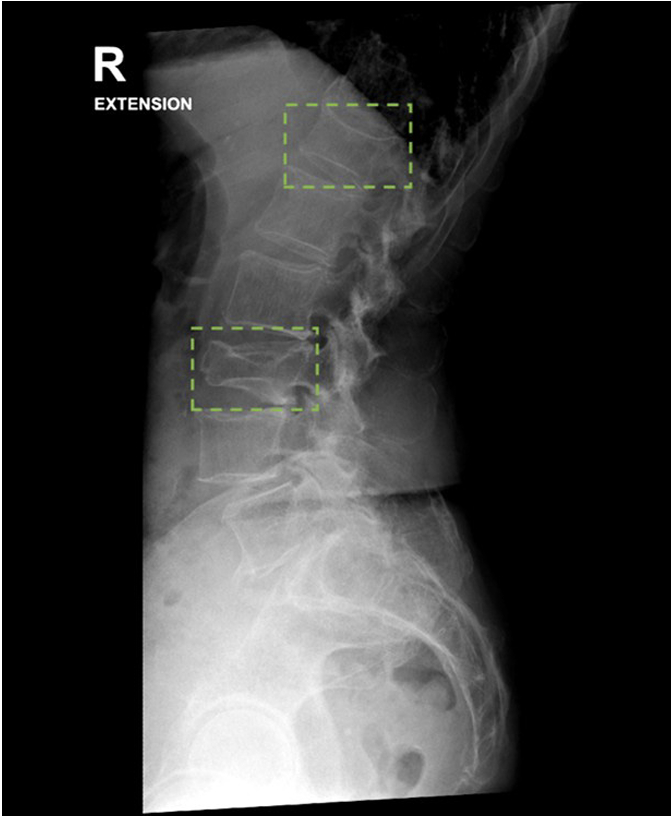
Figure 2: A) Largely unremarkable anteroposterior pelvic radiograph (left) with generalised reduced radiographic bone density and normal sacral appearances, and
B) coronal T2-weighted lumbar magnetic resonance imaging (right) shows bilateral linear regions of subchondral hyperintensity within the sacral alae, consistent with bone marrow oedema secondary to bilateral sacral insufficiency fractures (green arrows).

Notably, a single fragility fracture increases the likelihood of subsequent fractures two- to fourfold; up to 80% of patients diagnosed with a sacral insufficiency fracture has evidence of prior fragility fractures. Although asymptomatic at the time of orthopaedic review, the patient’s prior disabling pain episodes, oncologic history, and prior fractures warranted MRI investigation to consider occult pathology.
Management of SIFs extends beyond symptom control and requires a comprehensive, multidisciplinary approach to bone health.1,2 Best practice involves addressing modifiable lifestyle factors, optimising nutrition and vitamin D status, initiating appropriate pharmacologic therapy (including bisphosphonates), and managing
underlying medical comorbidities.
Bisphosphonates, such as intravenous zole dronate, pamidronate and oral alendronate, are commonly recommended for at least 3–5 years, and may be reassessed based on fracture risk, bone turnover markers and bone mineral density response. Evidence from a recent meta-analysis of 22 randomised controlled trials supports the use of bisphosphonates in improving bone mineral density, reducing the incidence of secondary fractures and improving quality of life in osteoporotic patients with fragility fractures. In cases of ongoing fracture risk despite standard therapy, referral to endocrinology is appropriate for further evaluation and treatment. Exercise-based rehabilitation presents an important opportunity for reducing falls risk and improving confidence and skeletal bone quality, even in older adults. Low-intensity weight-bearing strength training and balance-focussed exercises guided by physiotherapists should complement multidisciplinary coordinated care alongside general practitioners and endocrinologists in addressing fracture risk and osteoporosis.
Conclusion
SIFs should be considered in older adults with recurrent lumbopelvic pain, especially those with osteoporosis or cancer history. This case reinforces the limitations of plain radiography and the value of MRI in detecting occult fractures, and emphasises the role of timely, multidisciplinary care in reducing fracture-related morbidity.
Competing Interests
RVC reports support from the Health Research Council of New Zealand Clinical Research Training Fellowship paid via Auckland University of Technology. AHS reports consulting fees from ATEC Spine.
Acknowledgements
Written informed consent was gained for publication of this case report and use of medical imaging.
Author Information
Rohil V Chauhan:
Director and Orthopaedic
Physiotherapy Practitioner (Spine), Department of Orthopaedic Physiotherapy, Auckland Spine Surgery Centre;
Clinical Research Fellow, Auckland University of Technology;
Clinical Lecturer, Department of Exercise Sciences, The University of Auckland.
Amanjeet Toor:
Musculoskeletal Medicine Specialist, The
MSK & Pain Clinic, Auckland, New Zealand; Instructor, International Pain and Spine Intervention Society.
Anand H Segar:
Orthopaedic Spine Surgeon, Auckland City Hospital, Department of Orthopaedics and Auckland Spine Surgery Centre; Senior Lecturer, Faculty of Medical and Health Sciences, The University of Auckland.
Corresponding Author
Rohil V Chauhan:
Department of Orthopaedic
Physiotherapy, Auckland Spine Surgery Centre, 96E Carlton Gore Road, Newmarket, Auckland, New Zealand.
E: rohil.chauhan@hotmail.com
References
1. Rickert MM, Windmueller RA, Ortega CA, et al. Sacral Insufficiency Fractures. JBJS Rev. 2022 Jul;10(7).
doi:10.2106/JBJS.RVW.22.00005.
2. Lyders EM, Whitlow CT, Baker MD, Morris PP. Imaging and treatment of sacral insufficiency fractures. AJNR Am J Neuroradiol. 2010 Feb;31(2):201-210. doi: 10.3174/ajnr.A1666.
3. Tamaki Y, Nagamachi A, Inoue K, et al. Incidence and clinical features of sacral insufficiency fracture in the emergency department.
Am J Emerg Med. 2017 Sep;35(9):1314-1316. doi: 10.1016/j. ajem.2017.03.037.
4. Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000 Apr;15(4):721-739. doi: 10.1359/jbmr.2000.15.4.721
5. Bazell C, Hansen D, Pelizzari P, Pyenson B. Medicare cost of osteoporotic fractures [Internet].
Milliman; 2019 Sep [cited 2019 Aug]. Available
from: https://www.milliman.com/en/insight/2019/
Medicare-cost-of-osteoporotic-fractures
6. Sun J, Rahmati M, Xie W, et al. Efficacy and safety of zoledronic acid in the treatment of osteoporosis:
A meta-analysis of randomized controlled trials. Heliyon. 2024;10(13):e33871. doi: 10.1016/j. heliyon.2024.e33871.
7. Bae S, Lee S, Park H, et al. Position Statement:
Exercise Guidelines for Osteoporosis Management
and Fall Prevention in Osteoporosis Patients. J Bone
Metab. 2023 May 31;30(2):149-165. doi: 10.11005/
jbm.2023.30.2.149
