What is Greater Trochanteric Pain Syndrome (GTPS)? Anatomy and who gets it?
GTPS or lateral hip pain constitute a large number of musculoskeletal related presentations at the physician’s office1. GTPS is an umbrella term encompassing different clinical entities that may contribute to chronic intermittent lateral hip pain. Multiple labels such as “trochanteric bursitis” and “tronchanteritis” have been used in the past which is now regarded as a misnomer2. Invariably, the inflamed or enlarged bursa due to friction (sub-gluteal minimus/medius) is secondary or co-exist with an underlying pathology3. Gluteal tendinopathy is identified as one of the major culprits of GTPS along with iliotibial band (ITB) and tensor fascia lata (TFL) as potential causes3. Gluteal tendinopathy has a propensity for middle-aged women, between 40 and 60 years3 4. Large number of patients fail non-operative treatment with significant levels of dysfunction making important to find novel treatment strategies5. Pain tends to be localized to the bony greater trochanter with aggravating activities such as walking, stair climbing and lying on the affected side1.
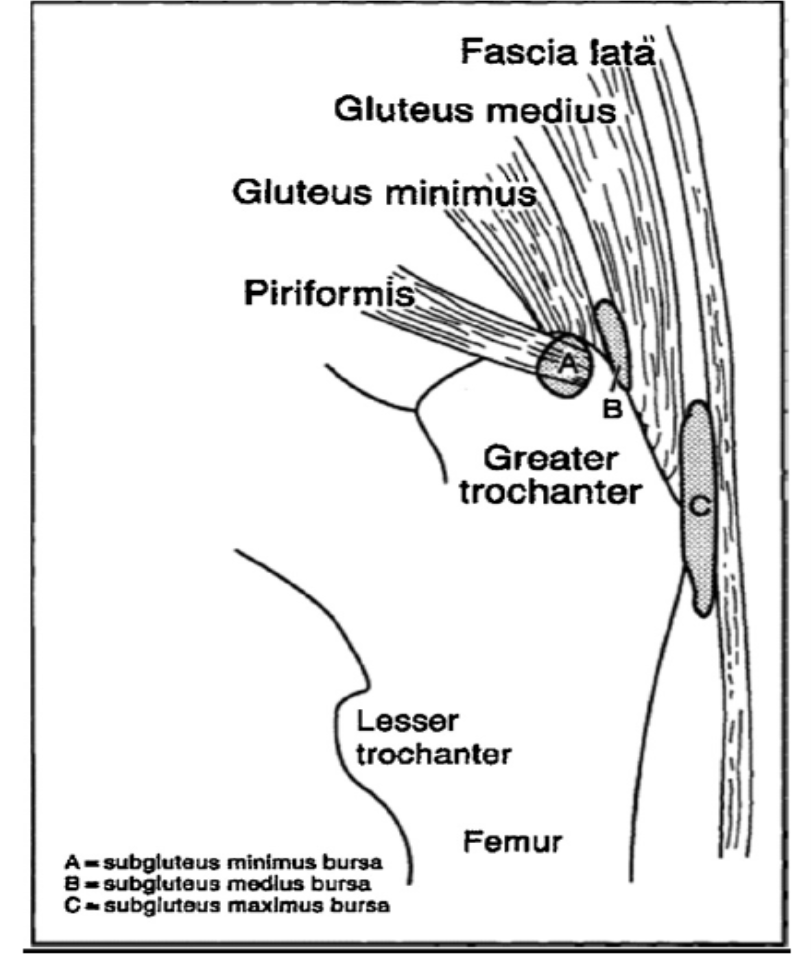
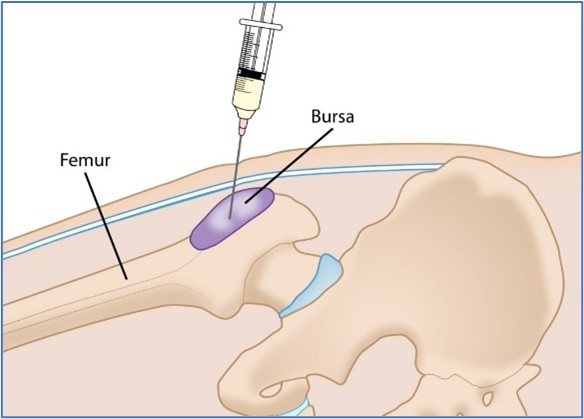
MRI and ultrasound are useful imaging tools to evaluate abnormalities of the lateral hip. Most clinicians use ultrasound guidance to inject medicine around the side of the hip bony protuberance. The liquid is deposited directly on the bone, around the tendons and some into tendon itself especially for PRP injections to stimulate cascade of cellular natural inflammation and healing process.
Current treatment options for GTPS
Acute cases (<3 months) tend to be responsive to conservative measures such as physiotherapy, eccentric stretching exercises, acupuncture, shock-wave therapy, CSI and NSAID2. CSI may provide benefit in the short term but with a high recurrence rate and poorer results in the long term5. Given the paucity of treatments for chronic gluteal tendinopathy (>3 months) and transient amelioration effect of CSI, there is interest whether biologic products such as PRP may provide better long term outcomes for this condition2 5. There is the consensus to reserve surgery only when conservative measures fail2. Systematic review by Koulischer et al (2015) pointed out that the time of onset of GTPS symptoms to surgery has declined over the years and still lack standardized surgical techniques for this condition2.
New emerging treatment- PRP
The use of PRP has been controversial, especially in tendinopathies given its slower onset of action to see its efficacy. Some tendons respond differently to PRP. Technician skills, type on condition being treated and type of PRP used are all variables that can affect its effectiveness.
What is PRP? How does it work?
Theory Behind It
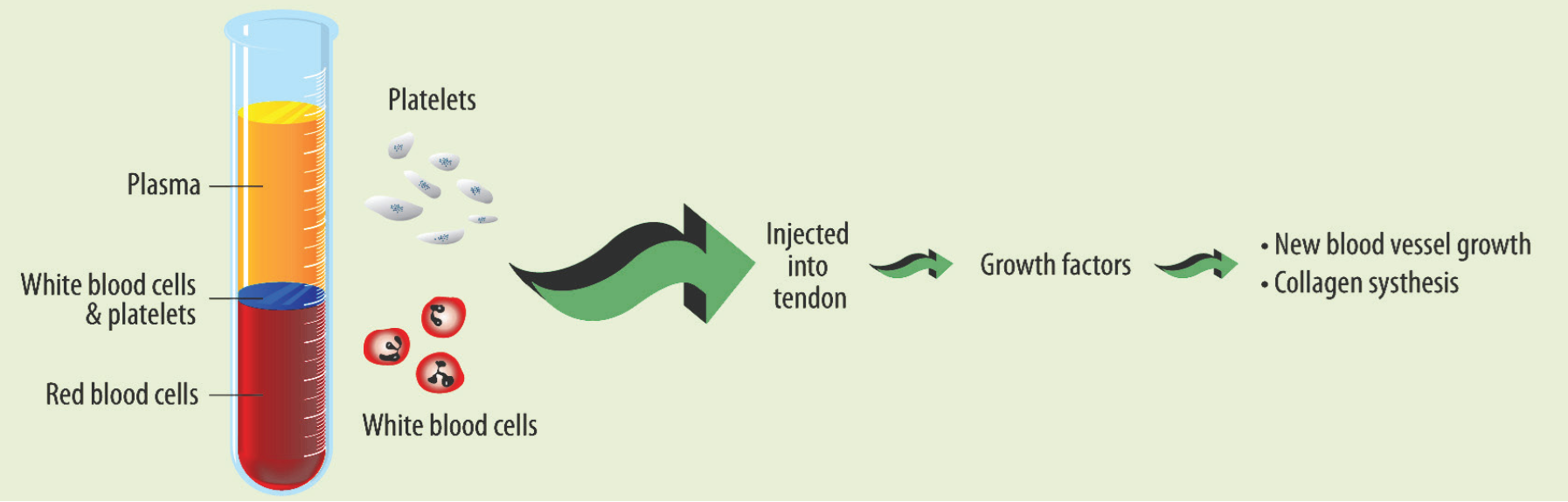
The aetiology of gluteal tendinopathy in GTPS has been proposed to be “failed healing” response. Ergo, lately ortho-biologics such as PRP has become popular in the musculoskeletal/orthopaedic community6. PRP is postulated to promote natural healing and provide a cocktail of high concentration cellular growth factors that mediate the regeneration tenocyte population in tendons3. Theoretically, the higher the concentration of platelets, the more growth factors will be present to promote healing at the desired area of injection6. PRP may often shorten rehab time and is an avenue to consider prior to considering surgery. High levels of platelets can be derived by centrifugation process of whole blood sample. FDA approved specific platelet harvesting centrifuge devices can increase the local concentration of platelets which is then injected into the target site7. Usually about 55 mLs of whole blood is extracted from the patient (from a vein in the elbow region) and mixed with anti-coagulant liquid in the centrifuge tube. This is then spun at high RPMs for 15- 30 mins depending on the centrifugation kit and desired PRP required by the clinician8. This process separate the blood components in order to discard elements not suitable (red blood cells which are heavy sink to the base), and to gather elements with therapeutic effects such as platelets, white cells, growth factors and fibrin8.
Common conditions treated with PRP
Common conditions treated with PRP – Lateral epicondylosis (tennis elbow), Medial epicondylosis (golfer’s elbow), Patellar tendinosis, Achilles tendinosis, Plantar fasciitis, Rotator cuff tendinosis, Gluteal tendinosis/Bursitis, Hip Labral tear, and Knee osteoarthritis.
Evidence for PRP
Below are some pragmatic studies done for the efficacy of PRP and other treatment modalities in GTPS. We encourage you to read this before making your decision:
Study
| Population | Year | Journal source | Conclusion |
Double-blind RCT LR-PRP for treatment of Chronic gluteal tendinopathy (> 4 months)5
| Follow up study at 2 years with 80 patients receiving either single PRP or corticosteroid injection (CSI) ultrasound (USS) guided. Cross-over allowed at 3 months. | 2019 | The American Journal of Sports Medicine 1–8 DOI: 10.1177/0363546519826969 | A single LR-PRP injection ultrasound guided results in greater improvement in pain & function than a single CSI at 2 years. |
Double-blind RCT LR-PRP for treatment of Chronic gluteal tendinopathy (> 4 months)1
| 80 patients receiving either single PRP or CSI USS guided. | 2018 | The American Journal of Sports Medicine 2018;46(4):933–939 DOI: 10.1177/0363546517745525
| A single LR-PRP injection ultrasound guided achieved greater clinical improvement than a single CSI at 12 weeks. No adverse events reported. |
Management of GTPS- systematic review2
| 11 studies included CSI, Shock-wave therapy, Home-exercises, Surgery | 2015 | Acta Orthop. Belg., 2015, 83, 205-214 | Positive effect for CSI in the first few months. Surgery poor outcomes after 6 months. Also, varying surgical techniques used and low study evidence. |
Management of GTPS- systematic literature review3
| 7 studies included (4 RCTs and 3 cohort studies) | 2016 | Journal of Orthopaedics 13(2016); 15-28 http://dx.doi.org/10.1016/j.jor.2015.12.006 | This paper pointed out on the low level of evidence done on surgical studies. Conservative management is still the main stay with 90% success rate. |
PRP in GTPS- systematic review6 | 4 RCTs, 5 case series | 2018 | Journal of Hip Preservation Surgery Vol. 5, No. 3, pp. 209–219 doi: 10.1093/jhps/hny027 Advance Access Publication 30 August 2018 | Improvement seen with PRP at 3- and 12-months post treatment. Relatively safe and effective. Lacks high quality studies. |
PRP in GTPS7
| Double-blind retrospective study done in NZ. | 2019 | NZMJ 13 December 2019, Vol 132 No 1507 ISSN 1175-8716 © NZMA www.nzma.org.nz/journal | No difference in PRP and placebo group. Nevertheless, small study and wide range of platelet concentration used (low concentrations?). |
Benefits and potential Side effects
PRP is an autologous preparation, thus inherently safe, free from allergenic and transmissible infection7.
This makes the procedure safe and easily reproducible. Moreover, PRP injection also carries less chance for infection than an incision, with a considerably shorter recovery time than after surgery. Previous studies have only identified transient post injection soreness as a potential side effect.
Accessibility and cost in NZ- who offers it?
PRP is often done by Musculoskeletal Medicine or Orthopaedic specialists within the private healthcare system. Some insurance companies might fund part of the procedure cost. A referral letter is required from your General Practitioner to the specialist service. The cost may vary from $500 to 750$ per injection depending on the type of PRP used and preparation process. Up to 2-3 injections maybe required to achieve maximal benefit depending on clinical response.
What to expect on the day of procedure?
After a consultation, if appropriate, the procedure can be done under ultrasound guidance in the clinician’s rooms, or in a local radiology suite. It is advised to wear loose clothing to allow adequate exposure of the injection site. Any anti-inflammatory or aspirin should be stopped one week before and four weeks after. Please check with your family doctor prior to stopping your aspirin.
Post- PRP injection Care:
- Pain- You might feel like a “bruise’ feeling 24-48 hours post-injection. Please call your doctor if you notice any numbness, redness, discharge, or fever.
- Driving- Depending on the area injected (e.g. heel/hip/knee), you might need someone to accompany you to drive you home after the injection.
- Activity- You should avoid strenuous activity for the first 48 hours.
- Work- Depending on the work you do; you might only need one day off on the day of the procedure.
- Follow up appointment- usually will be informed by your doctor/specialist.
- Concerns- call your family doctor or physician’s office who administered the PRP injection.
Post- PRP injection Rehab Protocol:
Treatment (Day)
| Regimen |
1 (1st PRP)
| RICE- Rest, Ice, Compression, and Elevation are important. Ice the treated area 20 minutes every 2 hours for the first 12 hours – avoid strenuous activity. |
2-6
| Passive stretches, light exercises, start using the joint/muscle at 20-30% of normal use. You may start normal exercise within pain limits. Ice at the end of the day. |
7 | Follow-up with your Specialist. |
8-13
| Slowly increase activity according to advice from specialist on strengthening the structure that was treated. |
14 (2nd PRP) | RICE regimen as aforementioned. |
15 onwards | Structured physio rehab. Might need 3rd PRP depending on response. |
Note: This regimen might vary depending on degree on pathology, patient response and physician advice.
Should I go for it?
The role of PRP in GTPS is open for debate. Nevertheless, some studies show promising results in the long term compared to corticosteroid injection and is a reasonable option if other conservative measures have failed.
- Fitzpatrick J, Bulsara MK, O’Donnell J, et al. The effectiveness of platelet-rich plasma injections in gluteal tendinopathy: a randomized, double-blind controlled trial comparing a single platelet-rich plasma injection with a single corticosteroid injection. The American journal of sports medicine 2018;46(4):933-39.
- Koulischer S, Callewier A, Zorman D. Management of greater trochanteric pain syndrome: a systematic review. Acta Orthop Belg 2017;83:205-14.
- Reid D. The management of greater trochanteric pain syndrome: a systematic literature review. Journal of orthopaedics 2016;13(1):15-28.
- Bancroft LW, Blankenbaker DG. Imaging of the tendons about the pelvis. American Journal of Roentgenology 2010;195(3):605-17.
- Fitzpatrick J, Bulsara MK, O’Donnell J, et al. Leucocyte-Rich Platelet-Rich Plasma Treatment of Gluteus Medius and Minimus Tendinopathy: A Double-Blind Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med 2019;47(5):1130-37. doi: 10.1177/0363546519826969 [published Online First: 2019/03/07]
- Ali M, Oderuth E, Atchia I, et al. The use of platelet-rich plasma in the treatment of greater trochanteric pain syndrome: a systematic literature review. Journal of hip preservation surgery 2018;5(3):209-19.
- Thompson G, Pearson JF. No attributable effects of PRP on greater trochanteric pain syndrome. The New Zealand Medical Journal (Online) 2019;132(1507):22-32.
- Ehrenfest DMD, Andia I, Zumstein MA, et al. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles, ligaments and tendons journal 2014;4(1):3.