Abstract
The knee joint is truly unique. Despite all the medical armamentariums in this modern world, there is no way of replicating the real biomechanics of the knee joint. The knee joint stability is contributed by a variety of anatomical structures which include bone, menisci, muscles, tendons, ligaments and the joint capsule. Any derangement in these structures can lead to poor biomechanics and subsequent injury risk. Anterior cruciate ligament (ACL) injury is frequently encountered in the sporting world. It is a severe and often career-ending injury with substantial health economic burden. Contact sports as the main culprit for ACL rupture is a false notion. ACL injury occurs commonly in non-contact sports with a predilection for young female athletes. The heterogeneity of the joint, i.e., tibial slope, intercondylar notch width and femoral condyle size all play a part in contributing to ACL injury. The author postulates the presence of knee joint anatomic variance, gender and type of sports are risk factors for ACL injury. Scrutinizing the knee biomechanics allows appropriate ACL injury prevention programmes to be put in place.
Clinical setting
The author is a musculoskeletal medicine doctor based at a hospital in Auckland, New Zealand. The case study involves Ms. R, a 20-year-old female who works as a business consultant. She was referred for further specialist care by her physiotherapist after failing to respond to conservative therapy. She was four months out from her injury at her specialist consult.
History of presenting complaint: Ms. R injured herself during hockey in February 2022. She twisted her left knee while making a sudden turn. She reported immediate knee pain and swelling within a few hours. Her aggravating factors included any loaded exercises especially lunges, and long runs. Resting alleviated her pain. Her pain was rated as five out of ten on the visual analogue scale (VAS). She denied systemic symptoms such as fevers, early morning stiffness or unintentional weight loss.
Past Medical History: Asthma, Coeliac’s disease, Migraines.
Medications: Pulmicort inhaler 1 puff twice daily, Ventolin inhaler PRN. Allergy- nil.
Social History: She drinks alcohol socially and is a non-smoker. Her usual exercise regimen involves gym sessions, hockey, running, and Karate.
Previous Investigations: Normal knee X-ray.
Examination: On examination, her lower limb alignment looked normal. Valgus alignment of 50. She had a normal gait and cadence. There was no knee joint effusion or muscle wasting. She was tender over the medial and lateral joint lines. Her knee joint range of motion was 0-1350 with normal patella tracking. Her cruciate and collateral ligaments were intact. McMurray’s test was negative. Her lower limb neurovascular status was intact distally.
Management: The author’s initial impression of Ms. R’s presentation was chronic somatic knee pain. There were no true locking or instability symptoms. The differentials included an internal knee joint derangement such as ACL injury, meniscal injury and/or minor bone contusion. Given the chronicity of her pain, a magnetic resonance imaging (MRI) scan of her knee was requested. Her MRI scan revealed a bone marrow trabecular injury of the lateral femoral condyle with small cartilage flaps in the anterior aspect of the lateral femoral condyle. The ACL was irregular and oedematous. She was advised to stay off strenuous activities and concentrate on non-impact activities such as static biking, cross trainer, and leg extension exercises.


Introduction
In the last few decades, the sporting world has grown with more female athlete participation(Patel, Hageman, Quatman, Wordeman, & Hewett, 2014). There has been a drastic increase in ACL injuries incurred by young athletes(Patel et al., 2014). Certain sports involving jumping and pivoting, and the female sex are now known as risk factors for ACL injury(Patel et al., 2014). The advancement of medical imaging such as MRI scans can detect ACL ruptures, and even subtle subchondral bone oedema(Patel et al., 2014).
Discussion
Anatomy of the Knee Joint
The knee joint is a structurally complicated structure with subtle anatomic variations amongst the population. It comprises two important intrinsic ligaments, i.e., the posterior and anterior cruciate ligaments. The medial and lateral collateral ligaments are the extrinsic ligaments. All of these ligaments play their roles respectively to provide knee stability. This paper looks specifically at ACL injury biomechanics and risk factors. The ACL is the primary knee stabiliser preventing anterior tibial translation on the femur and limits internal rotation(Balachandar, Marciniak, Wall, & Balachandar, 2017). The ACL extends from the lateral femoral condyle to the anterior tibial spine. Its inherent role in stabilising the joint is crucial especially, in tasks involving cutting and landing(Lopes et al., 2018). Invariably, ACL ruptures lead to post-traumatic knee arthritis and only about half of athletes return to competitive sporting level(Lopes et al., 2018).
Aetiology of ACL injury
Often ACL injuries occur when an athlete lands on one leg and pivots on the ground(Sonnery-Cottet et al., 2011). Risk factors can be caused by intrinsic and extrinsic factors(Sonnery-Cottet et al., 2011). Factors inherent to individuals such as intercondylar notch width, gender, neuromuscular imbalances, genetics and hormonal are intrinsic(Jha, Azam, Jain, & Bali, 2022). Type of sports, playing surface and weather are classified as extrinsic factors. The relationship between gender as a variable and risk of ACL injury is still not fully understood(Montalvo et al., 2019).
Studies frequently quote contact sports such as rugby and wrestling when comparing ACL injury risk in males and females. ACL injuries are thought to be prevalent in female athletes in limited or non-contact sports such as skiing, football, basketball and gymnastics(Montalvo et al., 2019). The figure below clearly depicts the different types of sports:
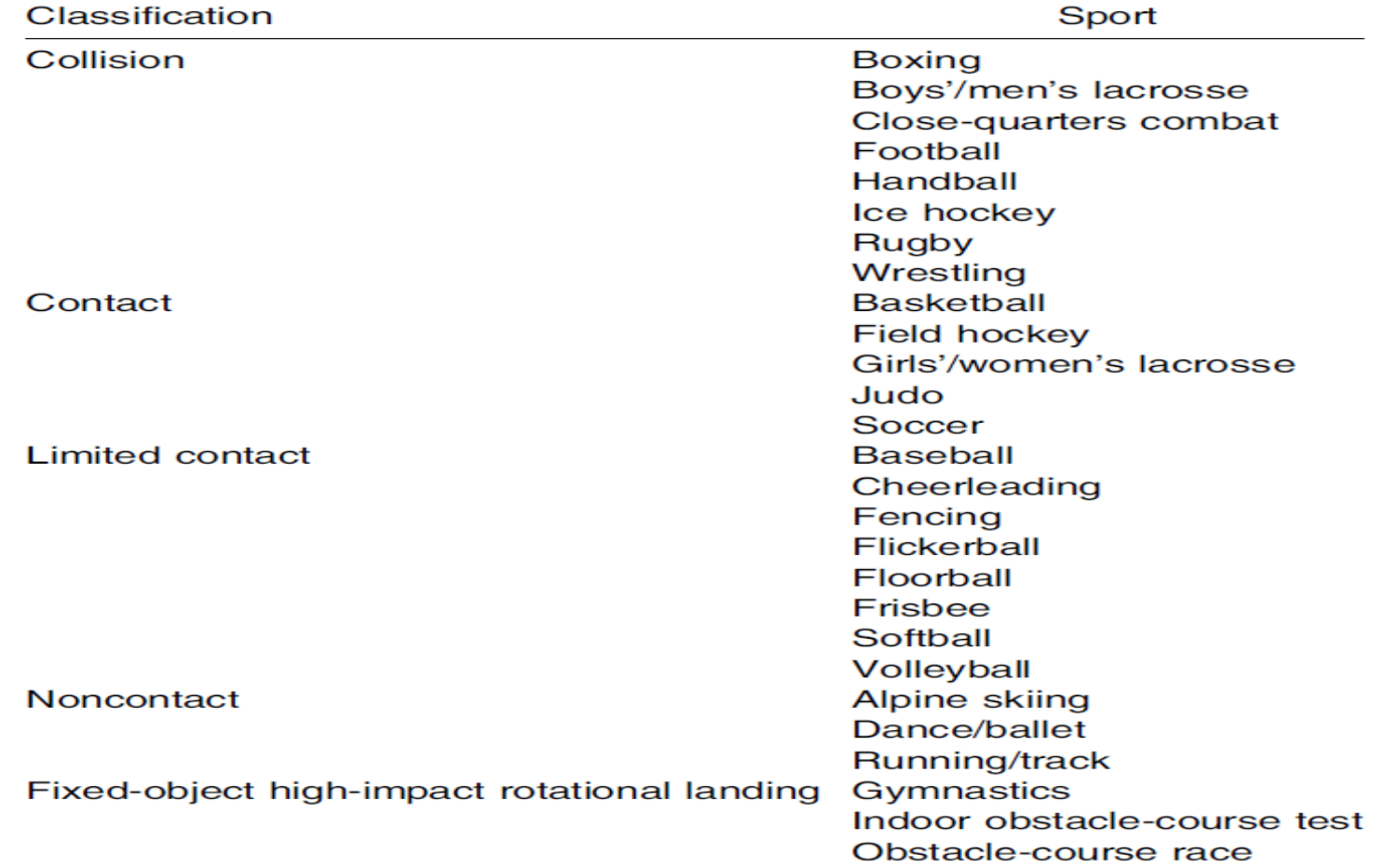
A robust systematic review and meta-analysis published in 2019 by AM. Montalvo and colleagues looked at sex differences in the incidence rates of ACL injury in different sports(Montalvo et al., 2019). They looked at different sports types which included collision, limited contact and non-contact type sports(Montalvo et al., 2019). Interestingly, the incidence rates of ACL injury were higher in females in contact sports. The researchers also studied sports categories involving fixed objects and high-impact rotational landings and found that female athletes were at greater risk(Montalvo et al., 2019). High-impact rotational landing, i.e., landing with a stiff leg and pivoting the lower leg pose a significant ACL injury risk(Montalvo et al., 2019). The study had some limitations. There was heterogeneity amongst the studies in the meta-analysis. There was also a lack of information in the studies regarding the surface type, and player hours as these were not the aims of the study(Montalvo et al., 2019)
Biomechanics and Risk factors for ACL injury
A recent paper published in the orthopaedic journal by Jha et al. studied 1,169 knees(Jha et al., 2022). The search yielded ten studies that were included in the analysis. They were mainly retrospective case-controlled studies in the last ten years(Jha et al., 2022). The main take-home message from the study was that ACL-injured knees have smaller femoral notch volume(Jha et al., 2022). This was similar for both the male and female sex. The plausible explanation for small notch volume being a risk factor is possibly a smaller and frail ACL. The other explanation is the risk of the ACL ligament getting impinged on the lateral femoral condyle as the tibia rotates causing shear stress(Jha et al., 2022). Again these are possibilities that are not proven. The clinical implication of this study is the ability to predict and stratify athletes(Jha et al., 2022). The low quality of evidence requires further research on notch volume.
Another paper published by Sonnery-Cottet et al. in 2011 looked at the combination of increased posterior tibial slope and a small intercondylar notch width as risk factors for ACL rupture(Sonnery-Cottet et al., 2011). There were two groups, i.e., 50 patients each in the ACL rupture and healthy control group. A high posterior tibial slope was defined as > 10.5 degrees and a tight notch ratio as < 0.21(Sonnery-Cottet et al., 2011). The study concluded that there was a correlation between ACL injury when both risk factors were taken into account rather than in isolation(Sonnery-Cottet et al., 2011). Nevertheless, there were some limitations in the study with small sample size and generalizability.
Nevertheless, there were some limitations in the study with small sample size and generalizability.


Another interesting point about ACL injuries is the bone bruise patterns. The current literature supports ACL injury as a valgus-driven mechanism(Patel et al., 2014). Often a bone bruise presents as a hyperintense signal on T2 weighted MRI scan imaging. A systematic review published in 2014 by Patel SA. and colleagues managed to review five papers that included bone bruise in their studies(Patel et al., 2014). The conclusion was bone bruise are common in the lateral compartment of the knee with ACL injuries(Patel et al., 2014). There was insufficient evidence to show a sex-specific bone bruise pattern(Patel et al., 2014). The author also highlighted the limitations of the study. The presence of concurrent injuries such as medial collateral ligament (MCL) sprain can confound the result. The time frame of an MRI scan is also crucial, i.e., between four to six weeks(Patel et al., 2014). Some of the patients in the study presented later than this.
Given that females are at higher risk of ACL injury, more studies are looking at hormonal mechanisms during the menstrual cycle. A systemic review by Balachandar V et al. in 2017 stated greatest risk for ACL injury is in the pre-ovulatory cycle where there is ligament laxity(Balachandar et al., 2017). Estrogen receptors are found on the ACL and lead to a decrease in fibroblast and type I collagen formation(Balachandar et al., 2017). Again these mechanisms are complex in themselves and the only plausible explanation to date is the increase of ACL laxity, ergo increasing injury risk. Consequently, this causes greater knee valgus and tibial external rotation(Balachandar et al., 2017).
More effort should be put into ACL injury prevention programmes since it is more achievable and has become quite popular amongst athletes. ACL injury prevention programmes aim at improving the landing biomechanics of the knee, for instance, reducing quadriceps dominance, increasing peak hip and knee flexion, and consequently reducing the peak knee abduction moment(Lopes et al., 2018). Petushek EJ. and colleagues conducted a comprehensive systematic review of ACL injury prevention guidelines in young female athletes(Petushek, Sugimoto, Stoolmiller, Smith, & Myer, 2019). In particular, they found specific neuromuscular training programmes targeting the lower body such as Nordic hamstrings, lunges, calf raises, and land-stabilisation activities are efficacious for ACL injury prevention(Petushek et al., 2019).
Conclusion
In conclusion, high force contact sports as a risk factor for ACL injury is a fallacy. There is a dearth of good literature establishing other risk factors such as female gender, small intercondylar notch, and sports involving high-impact rotational landing(Montalvo et al., 2019). The rationale behind studying risk factors is putting in place preventative strategies such as improving proprioception, muscle balancing (hamstring/quadriceps), and neuromuscular training to reduce ACL injuries in athletes(Sonnery-Cottet et al., 2011). The goal is to prepare athletes with avoidance techniques and perturbation is a pragmatic approach to mitigate the risk of ACL injury.
Reference
Balachandar, V., Marciniak, J.-L., Wall, O., & Balachandar, C. (2017). Effects of the menstrual cycle on lower-limb biomechanics, neuromuscular control, and anterior cruciate ligament injury risk: a systematic review. Muscles, ligaments and tendons journal, 7(1), 136.
Jha, V., Azam, M. Q., Jain, P., & Bali, S. A. (2022). Does femoral intercondylar notch volume differ in anterior cruciate ligament-injured adult patients compared to the uninjured?: a meta-analysis. Clinics in Orthopedic Surgery, 14(1), 76.
Lopes, T. J. A., Simic, M., Myer, G. D., Ford, K. R., Hewett, T. E., & Pappas, E. (2018). The effects of injury prevention programs on the biomechanics of landing tasks: a systematic review with meta-analysis. The American journal of sports medicine, 46(6), 1492-1499.
Montalvo, A. M., Schneider, D. K., Webster, K. E., Yut, L., Galloway, M. T., Heidt Jr, R. S., . . . Parikh, S. N. (2019). Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train, 54(5), 472-482.
Pacific Radiology PACS system. Auckland, New Zealand.
https://pacs.pacificradiology.com
Patel, S. A., Hageman, J., Quatman, C. E., Wordeman, S. C., & Hewett, T. E. (2014). Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Medicine, 44(2), 281-293.
Petushek, E. J., Sugimoto, D., Stoolmiller, M., Smith, G., & Myer, G. D. (2019). Evidence-based best-practice guidelines for preventing anterior cruciate ligament injuries in young female athletes: a systematic review and meta-analysis. The American journal of sports medicine, 47(7), 1744-1753.
Sonnery-Cottet, B., Archbold, P., Cucurulo, T., Fayard, J.-M., Bortolletto, J., Thaunat, M., . . . Chambat, P. (2011). The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. The Journal of bone and joint surgery. British volume, 93(11), 1475-1478.
