Abstract
The heterogeneity of the sacroiliac(SI) joint makes it a unique joint. Often discussed in medical textbooks, albeit overlooked in the real world. Despite all the clinical armamentarium in modern medicine, SI joint diagnosis is invariably misdiagnosed as lumbar discogenic or facet joint disease. This uncertainty leads to long-recognized paradox leading to a delayed diagnosis. It is imperative looking at the holistic picture of a clinical presentation and advocating good therapeutic care. Some of the conditions affecting this joint are inflammatory, trauma or mechanical dysfunction. This paper illustrates a SI joint pain case history, aetiology, and precision diagnosis with viable injection therapy options such as corticosteroid, prolotherapy (hypertonic glucose) and platelet rich plasma (PRP). Different fluoroscopic injection techniques and contrast dispersal in the SI joint are also discussed briefly to determine their relationship with pain abolishment. Other treatment options such as radiofrequency nerve ablation and surgical interventions are beyond the scope of this paper and therefore not discussed.
Clinical setting:
The author is based at a private practice hospital in Auckland, New Zealand working as a musculoskeletal medicine physician. The case history below involves Mrs S, a 70 year old retired Indian female who was referred by her physiotherapist for low back pain.
History of presenting complaint: She injured herself while gardening in a prolonged bent position. When she got up, she felt right low back pain. There was radiation of pain down the side of her right thigh and gluteal region. She denied radicular pain or paresthesiae in her lower limbs. Aggravating factors- bending, leaning forwards, sudden turns. Alleviating factors- physiotherapy exercises, resting on a flat surface. Her visual analogue scale(VAS) pain score on average was 4/10 and at worst 8/10. Her sleep was good and she was in good spirits. She denied any red flag symptoms of bladder, bowel, fevers or history of malignancy.
Past Medical History: Left total knee joint replacement (2008)- osteoarthritis, Gout, Hypertension.
Medications: Paracodeine 2 tabs twice daily, Allopurinol 300 mg daily, Amlodipine 5 mg daily.
Social History: Non-smoker. Teetotaler. Exercise- daily walks for 30 minutes.
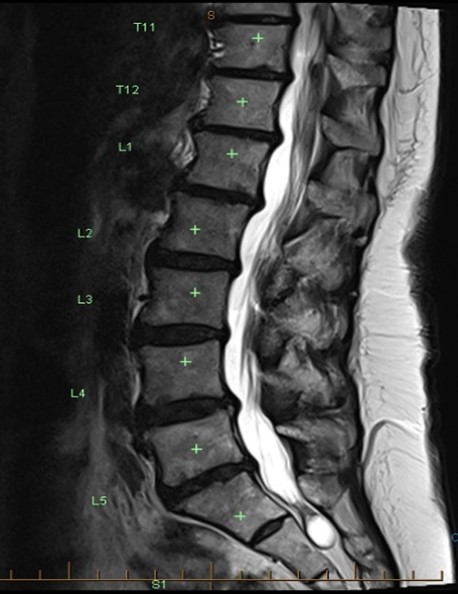
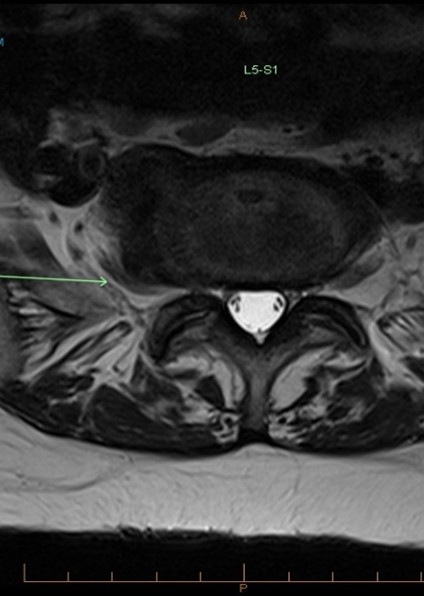
Previous Investigations: Xray lumbar spine showed lumbar spondylosis with marked disc height loss at L4/5 and L5/S1 levels. Mild degenerative disease at the sacroiliac joint articulation.
Examination: Sagittal and coronal alignment were normal. Gait and Trendelenburg test were normal. Tender right posterior superior iliac spine(PSIS). Lumbar flexion 500, extension 150. SLR up to 600– bilaterally negative. FABER(flexion, abduction and external rotation) test was positive. Other sacral provocation tests were positive (pelvic distraction/lateral compression/sacral anterior thrust/Gaenslen’s tests). Finger fortin test- right PSIS region. Hip joints pain were unremarkable. Lower limb neurology was normal.
Management:
The initial impression was right sacroiliac joint pain given her clinical examination findings and age. She was referred for a lumbar MRI which showed L4/5 and L5/S1 disc protrusions contacting the exiting L4 and L5 nerve roots, and SI joint degenerative changes. Due to clinical suspicion of SI joint origin pain, she underwent fluoroscopic guided right SI joint corticosteroid injection. Her pre-injection VAS pain score was 80/100 and five minutes post injection VAS 0/100. This was a positive block.
Introduction
Musculoskeletal medicine is a fascinating field evidenced by the myriad of clinical presentations. Clinicians usually postulate a list of differential diagnosis for low back pain. Low back pain is a common presentation which has progressed unabated over the last few decades(Chauhan, Hehar, Loomba, & Upadhyay, 2019). The SI joint can be a source of pain in about 15-30% of people presenting with unilateral gluteal or low back pain below the L5 level with a preponderance amongst older people(Chauhan et al., 2019; Saunders, Cusi, Hackett, & Van der Wall, 2018). The role of surgery is scrutinized these days due to the absence of its utility for pain relief itself(Saunders et al., 2018). The SI joint can be a primary source of mechanical pain or be involved in a syndromic condition such as ankylosing spondylitis or other inflammatory diseases(Chauhan et al., 2019). SI joint pain can be mimicked by other possible sources such as facetogenic pain, lumbar disc prolapse or gluteal tendinopathies(Chauhan et al., 2019). Physical examination manoeuvres can help narrow down the possible sources but none of these tests are pathognomonic(Chauhan et al., 2019). The ability of a clinician to dissect the different types of pain around the lower back, gluteal and thigh region confers benefit to avoid misdiagnosis and poorer medical care.
Discussion
Aetiology and Anatomy of the Sacroiliac Joint
The anatomic variation of the SI joint makes it difficult for nerve blocks and often needs intraarticular injection to anesthetize the joint(Chauhan et al., 2019) . The current literature supports the use intraarticular joint blocks as diagnostic test(Chauhan et al., 2019). Due to disparate anatomy, there is high numbers of incorrect injections leading to poorer success rates(Chauhan et al., 2019). Past studies have shown higher success with fluoroscopic guided intraarticular injections(Chauhan et al., 2019). Pain physicians are motivated in finding better techniques to improve reliability and validity(Chauhan et al., 2019).
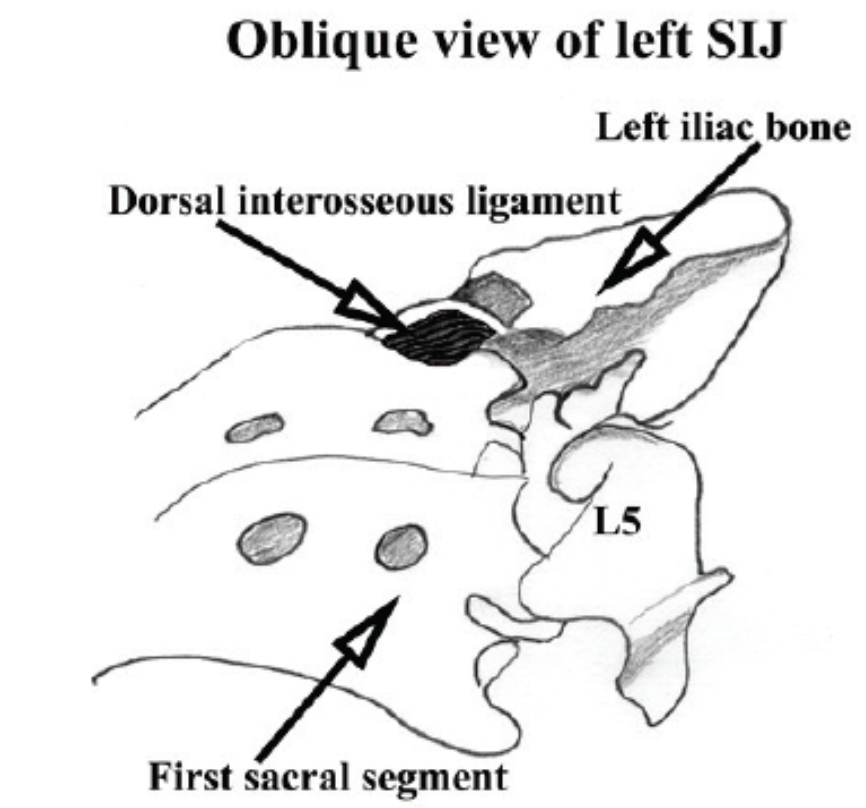
Cadaveric studies have shown the SI joint is a diarthrodial joint with the anterior part being a true synovial joint and posterior part lacking a joint capsule(Chauhan et al., 2019; Poilliot, Zwirner, Doyle, & Hammer, 2019). The posterior joint is often composed of fibrocartilage and thick ligaments such as the interosseous ligament, long posterior SI ligament and dorsal SI ligament(Chauhan et al., 2019). The dorsal SI joint ligament is composed of a superficial and deep part running in different directions to maximise SI joint stability(Saunders et al., 2018). It is considered one of the strongest ligaments in the body given the shear forces that it transmits from the spine to the pelvis(Saunders et al., 2018).
Hypothetical evidence has shown that pain can be generated from the SI joint or the dorsal SI ligamentous complex. A systematic review by Poilliot AJ . et al. studied the SI joint anatomy and surrounding tissues(Poilliot et al., 2019). This included 88 papers with a timeline from 1851 to 2018(Poilliot et al., 2019). They found the anterior part of the SI joint is supplied from the L4 to S2 segmental levels and possibly the superior gluteal nerve, whereas the posterior part is innervated by the lateral branches of dorsal rami of segments L5 to S4(Poilliot et al., 2019). In addition, there was asymmetry between both sides. The study also concluded that there was inconclusive evidence on SI joint sacral articulation and fatty tissue presence in the joint space(Poilliot et al., 2019) making the SI joint a truely enigmatic structure(Poilliot et al., 2019).
Diagnosing Sacroiliac Joint Pain: Treat the Patient not the Imaging
Laslett M. and colleagues studied a list of SI joint provocation manoeuvres to help with clinical diagnosis of SI joint pain(Laslett, Aprill, McDonald, & Young, 2005). The tests they included were the sacral thrust, lateral compression, distraction, thigh thrust, FABER and Gaenlen’s tests(Laslett et al., 2005). A combination of two out of four, or three out of five was found to be valid for the diagnosis of SI joint pain(Laslett et al., 2005). Clinicians should be wary with over prescribing investigations such as CT SPECT. This may light up as a “hot spot” on certain areas of the spinal column and pelvis but nonetheless does not validly indicate the source of pain. To date, the only valid diagnostic process to differentiate sacroiliac intraarticular joint pain and ligamentous origin pain is injection therapy. This has become the gold standard for diagnosis and treatment. There is some emerging evidence on radiofrequency ablation of the lateral branches of the dorsal rami of L4 to S3 nerves but there is no concrete evidential research(Poilliot et al., 2019). Furthermore, due to the anatomic variance of the joint innervation, this it not feasible for definitive invasive treatment. Ergo, injection therapy has become favourable for SI joint pain treatment.
Injection Therapy for Sacroiliac Joint Pain
There are few inherent techniques and approaches to diagnosing and treating SI joint pain. The other challenging aspect of SI joint pain is hypothetising the origin of the pain whether is from the ventral or dorsal SI ligamentous complex, or the SI intraarticular joint itself. Other inherent factors with different imaging modalities such as ultrasound or fluoroscopic guidance can affect the accuracy of intraarticular needle placement. Poorly placed needle at the target site can result in poorer outcomes. Three commonly used injection therapies are corticosteroid, prolotherapy and PRP. The logic of prolotherapy is stimulating natural inflammatory response of tissues whereas PRP provides higher concentration of platelets and growth factors directly at the site of interest, thus enhancing natural healing.
A paper published in 2018 by Saunders J. and colleagues looked at PRP and prolotherapy for the treatment of dorsal SI ligamentous complex pain(Saunders et al., 2018). This was a fairly small study that included 45 patients in two different treatment groups. The PRP preparation was fairly simple with 9 mL of blood centrifuged for five minutes at 3500 rpm and then injected via ultrasound guidance in the prone position(Saunders et al., 2018). There was only 1.6 times increase in platelet concentration from the baseline(Saunders et al., 2018). Although, both groups had improvement, the PRP group had significant improvement at three months and required less injections on average(Saunders et al., 2018). The pain scores improved in all performance indicators(Saunders et al., 2018). One of the salient features of PRP is the skill and cost of administrating it. Nevertheless, PRP and prolotherapy show promising results in the long term treatment for SI joint and dorsal SI ligamentous pain.
A systematic review by Ling JF. of five studies looked at PRP and corticosteroid injections for SI joint arthropathy(Ling, Wininger, & Hirase, 2021). These included one randomized level I evidence, two randomized level II studies, and two non-randomised level III studies(Ling et al., 2021). These studies measured pain scores up to six months. On the whole, there was a drop in VAS pain scores for both PRP and corticosteroid groups(Ling et al., 2021). There was some evidence PRP conferred more long term benefit compared to corticosteroid up to six months improvement(Ling et al., 2021). The limitations of this systematic review was inclusion of lumbar spondylosis as a diagnosis and the missing information on PRP centrifugation preparation in the selected studies(Ling et al., 2021). Furthermore, there was significant variation in PRP preparation between the studies.
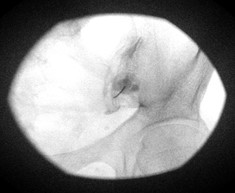
Chauhan G. and colleagues conducted a randomized double-blind controlled trial comparing the classic oblique approach to posteroanterior approach(Chauhan et al., 2019). They assessed the total procedure time and patient pain outcomes(Chauhan et al., 2019). With the newer posteroanterior technique, the C-arm was angulated in a 5-15 degrees cephalic tilt allowing greater visualization of the inferior portion of the SI joint(Chauhan et al., 2019). Patient selection was based on a simple and sensible criteria, a positive Patrick’s or Gaenslen’s tests, and had no pain above the PSIS level. The study concluded that the new modified posteroanterior approach had lower radiation exposure time and VAS pain scores post procedure(Chauhan et al., 2019). Nevertheless, the study had some limitations such as small sample size of thirty patients.
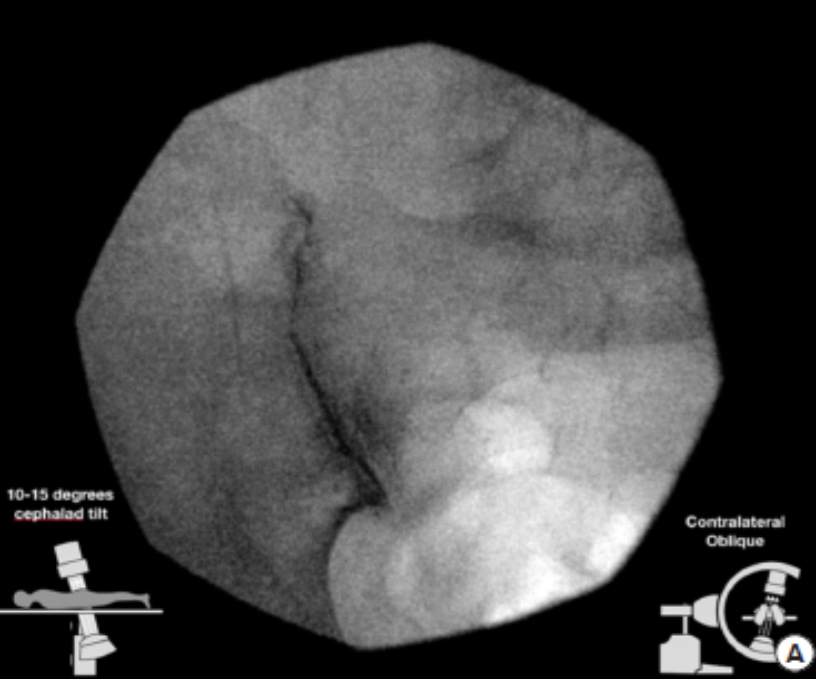
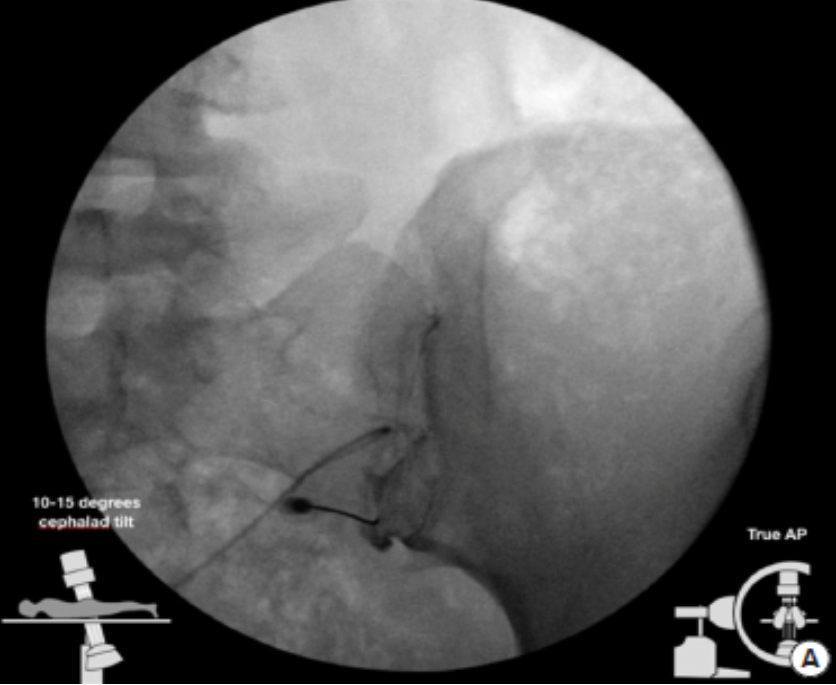
Scholten PM. et al. in his retrospective study looked at fluoroscopic contrast patterns in 49 subjects(Scholten, Patel, Christos, & Singh, 2015). In particular, interest was put into contrast flow patterns in the cephalad direction extending into the superior part of the SI joint(Scholten et al., 2015). The pain scores at two weeks were better in the cephalad extension group compared to the poor cephalad extension, though scores were similar in both groups at eight weeks(Scholten et al., 2015). This suggest it is important to have superior extension of corticosteroid liquid into the upper part of the SI joint to have better outcomes. Interestingly, the secondary measure looked at positive SI joint provocative tests. They found that in patients with at least one positive manoeuvre benefited from a SI joint injection(Scholten et al., 2015). Some of the limitations in this study were a small study population without a control group, and potential bias due to single blinded(Scholten et al., 2015).
A comprehensive systematic review by Simopoulos TT. and colleagues looked at diagnostic and therapeutic effectiveness of SI joint procedures(Simopoulos et al., 2015). The prevalence of SI joint pain was 15-30% based on controlled blocks with at least 70% pain relief(Simopoulos et al., 2015). These were level II studies for the diagnostic blocks. For the therapeutic effectiveness, consist mainly of Level III studies showed short term relief of pain with intraarticular corticosteroid injection and longer relief with prolotherapy(Simopoulos et al., 2015). Fluoroscopic guided injections had better accuracy and results compared with ultrasound guided.(Simopoulos et al., 2015). There was some evidence combined peri-articular and intraarticular injections of the dorsal SI ligaments had better results than just intraarticular injection by itself at three months(Simopoulos et al., 2015). Dual controlled blocks had fewer false positive results(Simopoulos et al., 2015). The limitations of this systematic review was the paucity of good quality diagnostic studies and variability in technique and inclusion criteria for therapeutic interventions(Simopoulos et al., 2015). All in all, using a stringent criterion standard of diagnostic blocks with at least 80% pain relief yields less false positive rates(Simopoulos et al., 2015).
Conclusion
Diagnosing SI joint as the source of pain can not only be challenging, but elusive(Simopoulos et al., 2015). Due to its heterogeneity,there is no single clinical exam or radiological test that can confirm the diagnosis of SI joint pain(Chauhan et al., 2019). There is dearth of good literature on sacroiliac joints which makes it difficult for clinicians to extrapolate information for better diagnosing and treating this joint. The only gold standard is diagnostic blocks. The notion that all low back pain is discogenic or facetogenic origin is a fallacy.This is a cardinal sin in the musculoskeletal medicine world. Precision diagnosis can be undertaken via injection therapy such as image guided corticosteroid, prolotherapy or PRP injections. A test only has true pragmatic value in a study if it is closely related to the clinical symptoms studied and management in clinical practice(Simopoulos et al., 2015). There is substantial evidence fluoroscopic guided PRP or prolotherapy injection provide long term benefit. However, there is a need for larger well-designed randomized controlled trials for future research.
Reference
Chauhan, G., Hehar, P., Loomba, V., & Upadhyay, A. (2019). A Randomized controlled trial of fluoroscopically-guided sacroiliac joint injections: a comparison of the posteroanterior and classical oblique techniques. Neurospine, 16(2), 317.
Laslett, M., Aprill, C. N., McDonald, B., & Young, S. B. (2005). Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther, 10(3), 207-218. doi:10.1016/j.math.2005.01.003
Ling, J. F., Wininger, A. E., & Hirase, T. (2021). Platelet-Rich Plasma Versus Corticosteroid Injection for Lumbar Spondylosis and Sacroiliac Arthropathy: A Systematic Review of Comparative Studies. Cureus, 13(3), e14062. doi:10.7759/cureus.14062
Poilliot, A. J., Zwirner, J., Doyle, T., & Hammer, N. (2019). A Systematic Review of the Normal Sacroiliac Joint Anatomy and Adjacent Tissues for Pain Physicians. Pain Physician, 22(4), E247-E274.
Saunders, J., Cusi, M., Hackett, L., & Van der Wall, H. (2018). A comparison of ultrasound guided PRP injection and prolotherapy for mechanical dysfunction of the sacroiliac joint. J Prolotherapy, 10, e992-999.
Scholten, P. M., Patel, S. I., Christos, P. J., & Singh, J. R. (2015). Short-term efficacy of sacroiliac joint corticosteroid injection based on arthrographic contrast patterns. Pm r, 7(4), 385-391. doi:10.1016/j.pmrj.2014.10.007
Simopoulos, T. T., Manchikanti, L., Gupta, S., Aydin, S. M., Kim, C. H., Solanki, D., . . . Hirsch, J. A. (2015). Systematic review of the diagnostic accuracy and therapeutic effectiveness of sacroiliac joint interventions. Pain Physician, 18(5), E713-756.
Specialist Radiology Group (SRG) PACS system. Auckland, New Zealand. https://pacs.srgmri.co.nz
